 Every state has its own Medicaid program. In Virginia, the Medicaid program has three different levels of benefits. In addition to the Medicaid program, there is also a program called FAMIS that might be helpful. Both are Medical Assistance Programs.
Every state has its own Medicaid program. In Virginia, the Medicaid program has three different levels of benefits. In addition to the Medicaid program, there is also a program called FAMIS that might be helpful. Both are Medical Assistance Programs.
Medicaid is a public, or government run, form of health insurance coverage. It is designed to provide health insurance coverage for individuals and families who are low-income, and who cannot afford to purchase a health plan from a private insurance company. Medicaid is funded, in part, by the federal government. It is also funded, in part, by the government of an individual state.
The Medicaid program in Virginia is administered by the Virginia Department of Medical Assistance Services (DMAS). Another department, the Department of Social Services (DSS) is responsible for taking applications and for determining eligibility.
To apply for Medicaid in Virginia, you need to contact the Department of Social Services in the city or county where you live. This state does not require a face-to-face interview in order for you to apply. You must fill out the Medicaid application and sign it.
You will also be asked to provide certain types of information. You must provide your Social Security number. You have to confirm that you are a resident of the state of Virginia. You also have to provide proof of United States citizenship or documentation of alien status. You will be expected to verify your income and resources. You also have to submit your bills for medical services that you received in the past three months.
Medicaid is designed to cover people who fit into the following groups: pregnant women, children, people who are age 65 or older, and people who have disabilities. The person must fit into the income limitations, and be able to provide the information described above.
The Medicaid program in Virginia has three levels of benefits. “Full Coverage” provides the full range of benefits. This includes doctor, hospital, and pharmacy services for those individuals not enrolled in Medicare.
“Time-limited Coverage” will cover people who do not meet the income limitations of Medicaid, but who do meet the requirements for a spenddown. It is also for women who have given birth and who want to receive 24 months of family planning services after their Medicaid coverage expires.
“Medicare-related Coverage” provides Medicaid payment of a person’s Medicare premiums. It may also cover payment of the Medicare deductible and co-insurance, up to Medicaid’s maximum payments. This level of coverage is for people who are covered by Medicare and who are having difficulty making the payments associated with that program.
FAMIS stands for Family Access to Medical Insurance Security Plan. It has different financial and non-financial eligibility requirements than the main Medicaid program does. This could be an option for families who need help with health insurance coverage but do not qualify for Medicaid.
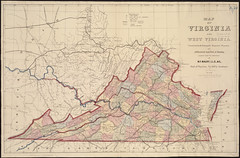
Image by Normal B. Leventhal Map Center at the BPL on Flickr

