 Postpartum depression affects roughly one in 8 women and is much more than a feeling of unhappiness or sadness. It is a real illness, is beyond the mother’s control, and requires medical intervention.
Postpartum depression affects roughly one in 8 women and is much more than a feeling of unhappiness or sadness. It is a real illness, is beyond the mother’s control, and requires medical intervention.
Postpartum depression may develop as a result of a pre-existing depression which worsens after birth, or it may come entirely out of the blue. The condition may occur immediately after the birth, develop suddenly in the days and weeks following the birth. Alternatively, it may slowly manifest over a period of weeks and months so that mother and family alike are initially unaware of the presence of the disorder until it is well established.
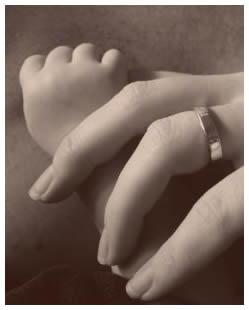
Mother-baby bonding may be temporarily interrupted due to the presence of postpartum depression. It is rare that the mother is so unwell that bonding cannot occur at all. More commonly the mother’s condition fluctuates on a daily, even hourly basis, and makes for difficulties as the mother generally feels unable to cope with the heavy demands of being a full-time carer of the new infant.
Although you as a mother may feel withdrawn from your baby and feel no desire at times to even see or deal with your baby, it does not mean that your maternal feeling are absent or in some ways “damaged”. They are still there, just obscured by the cloud of depression. Simply knowing that you are suffering from an illness, and that illness is causing you to behave in ways that you would never dream of behaving, can help mothers to cope better with both their babies and the condition alike.
It is also important to remember that you as a mother have little control over the feelings you are experiencing and that in time, and with adequate treatment, you will recover. Yet there will still be times that you feel you have nothing to give: remember this is not the real you. This is the illness. It is the same as if you had influenza, and were unable to care for your baby. Postpartum depression is a real condition and has real symptoms. It is simply not possible at this stage of the illness to “pull your socks up.” You should not expect yourself to be able to do so, nor should you take on board that same advice from a well-meaning friend or relative.
Depressed mothers often make life harder by berating themselves for their inability to be “good mothers,” whatever that concept means to them. If antidepressants are prescribed and breastfeeding is discontinued, it is very common for depressed mothers to become even more distressed due to their perceived inability to “even feed their own babies.” Again, this is the depression talking. Once the depression lifts, these thoughts of despair and lack of belief in your own abilities will vanish, and be replaced by the usual range of maternal feelings, including love, pride, tiredness, frustration, and joy.
Women suffering from postpartum depression therefore need constant reassurance that all will be well once the depression has lifted. In the next blog, we will discuss how best to care for mother and child, preserving the mother/child bond during this difficult time, and helpful hints for the father and other family members.
Contact Beth McHugh for further information or assistance regarding this issue.

